Are you looking to get an extension on your ACA filing?
Although the March 31st due date has come and gone, it's still helpful to know about the extension process so you can prepare for next year — or assess your penalties for this year.
So, let's take a look at what is required to file an extension and what happens if you don't.
ACA Filing: Who Is Required to Report?
The Affordable Care Act (ACA) was passed in 2010 to expand health coverage, improve healthcare quality, and change insurance industry regulations.
Since its passing, Applicable Large Employers (ALEs) have been required to report ACA data to the IRS each year.
To qualify as an ALE by IRS standards, a company must have 50 or more full-time or full-time equivalent employees (FTEs). Full-time employees are those who work at least 130 hours per calendar month.
Full-time equivalent employees are a combination of non-full-time employees who collectively work the same hours as full-time employees.
To determine how many full-time equivalent employees you have, you'll have to add up the hours for employees who worked less than 30 hours a week or 130 hours a month. Then, divide that by 120 to determine how many FTEs you have for that month
If the above calculation results in 50 or more full-time employees, then ACA data is required. If it's less, then ACA filing is usually not required.
Reporting Requirements for ACA Filing
The Employer Shared Responsibility Provisions (ESRP) of the ACA — also called the "employer mandate" or "pay or play provisions" — stipulate that ALEs need to provide minimum essential coverage (MEC) to 95% of their full-time employees and dependents.
MEC requires affordability and minimal value.
Affordability (at least in 2022) means that health coverage doesn't cost more than 9.61% of an employee's annual income. To determine what's affordable, employers can defer to three "safe harbors": the federal poverty line, rate of pay, and W-2 forms.
Minimum value means the health insurance must cover at least 60% of common health care costs.
ALEs need to prove they provide MEC to employees by filing two main forms with the IRS: 1095-C and 1094-C.
1095-C is the "Employer-Provider Health Insurance Offer and Coverage" form. It's furnished (i.e. handed out) to employees and then filed (i.e. sent) to the IRS.
1094-C is the "Transmittal of Employer-Provider Health Insurance Offer and Coverage Information Returns." It's filed alongside the 1095-C forms to provide the IRS with a summary of the ACA data in those forms.
Compliance Deadlines for ACA Filing
There are two main kinds of compliance deadlines to be aware of when doing your ACA filing. The first is federal, and the second is state level.
Federal Compliance Deadlines
The following three federal guidelines are important to keep in mind:
- February 28th: deadline for filing paper 1095-C and 1094-C forms
- March 2nd: deadline for furnishing employees with their 1095-C forms
- March 31st: deadline for e-filing 1095-C and 1094-C forms
It's important to note that any ALEs with 250 or more employees must do electronic filing. Also, if any of those compliance deadlines fall on a weekend or holiday, then it moves to the next business day.
State Compliance Deadlines
Alongside federal reporting requirements, California, Rhode Island, New Jersey, Massachusetts, and Washington, D.C. all have separate state-level reporting requirements. Their deadlines are as follows:
- California: March 31st to file 1095-C and 1094-C
- Rhode Island: March 31st to file 1095-C
- New Jersey: March 31st to file Form 1095-C
- Massachusetts: March 31st to file Forms 1099-HC
- Washington, D.C.: April 30th to file Form 1095-C
How to Get an ACA Filing Extension
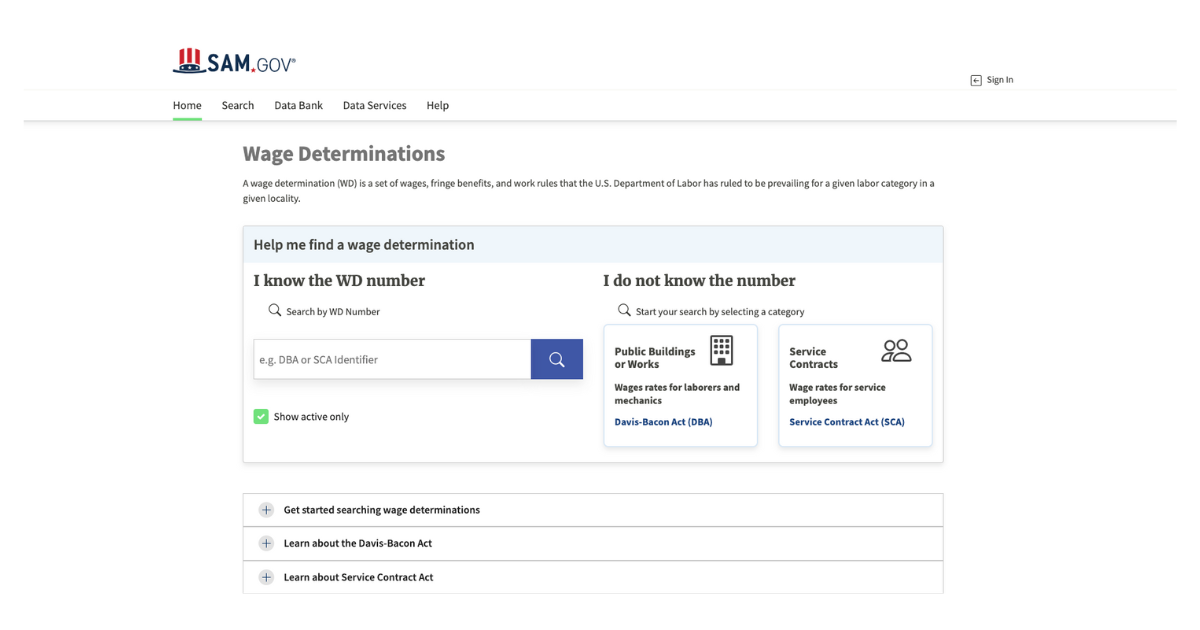
If your ALE fails to meet the compliance deadlines above, it's possible to request a 30-day extension.
You can do this by filling out Form 8809— the "Application for Extension of Time to File" — before the March 31st deadline. Although the IRS doesn't guarantee a 30-day extension, they generally approve of them. However, they may require more details on why you need the extension.
If you forget to file Form 8809 before the deadline, it's still important to file your forms as soon as possible. The penalties for filing late are less harsh than the penalties for not filing at all.
Late Penalties for ACA Filing
The penalties for late ACA filing fall into two categories: failure to furnish and failure to file.
Failure to furnish means not giving employees the 1095-B or 1095-C forms by March 2. Penalty amounts change from year to year, but for 2022 it was $280 per return.
Failure to file means not filing ACA data to the IRS in an accurate and timely manner. Again, penalties change slightly from year to year, but for the 2022 taxable year, it was $280 per return. However, if the IRS determines that the failure was caused by blatant disregard, then they may double the penalty to $560 per return.
The sooner you file, the better. Generally speaking, the IRS reduces fines for ALEs who are less than 30 days late versus those who are more than 30 days late.
Stay on Top of ACA Filing with Points North
Missing the regular compliance deadlines for ACA filing can be nerve-wracking. Missing the 30-day extension period is even more so. The best way to avoid both of those situations is to stay on top of ACA data gathering during the year.
Through their ACA Reporter software, Points North has been helping ALEs all over the country keep up to date with their reporting requirements so they can avoid late penalties. If you're concerned about late filings or keeping on top of all the ACA requirements, then contact Points North today to see how we can help.


.png)